Vasopressors
The cognitive response to hypotension should not be reaching for a pressor. The primary therapy for any sick hypotensive patient is treatment of the underlying pathology - Anand Swaminathan MD
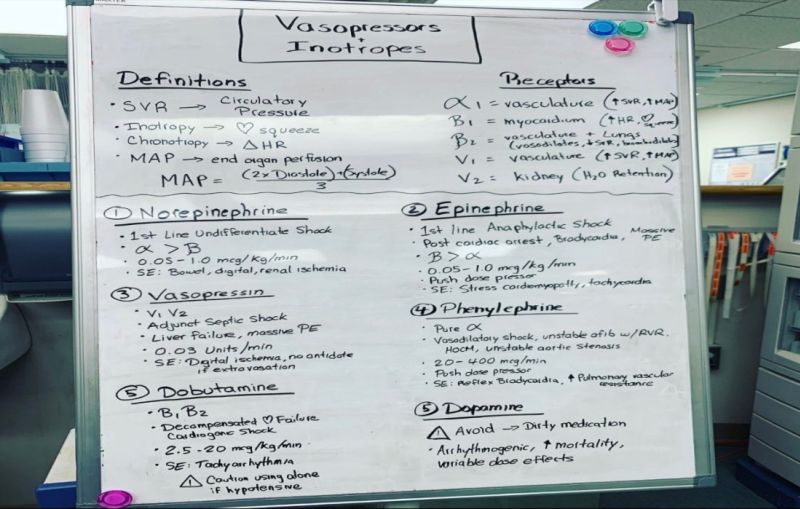
image by: Medicine Training in the US
HWN Recommends
Peripheral Vasopressors – Are my days of Placing Central Lines Over? Not Yet?
You have undoubtedly heard some discussion about data coming out over the last couple of years suggesting the risk of running vasopressors via peripheral IV's is less than we previously thought.
Well I'm here to tell you: don't let your central line skills erode just yet. While new studies that change our practice are exciting, we must be careful not to be early adopters after reading just the headlines.
Resources
 Peripheral Vasopressors: Do I need that central line?
Peripheral Vasopressors: Do I need that central line?
Peripheral administration of vasopressors has classically been reserved for less potent vasoconstrictors such as phenylephrine and vasopressin. Fear of extravasation and tissue injury often is a cause for concern prior to starting norepinephrine, epinephrine or dopamine peripherally. The perceived harm from administrating these medicines peripherally largely stems from case reports over the past 60 years.
 Cardiogenic Shock: Which Vasopressor to use
Cardiogenic Shock: Which Vasopressor to use
In the patient who presents with cariogenic shock, the cath lab and a stent or a CABG is probably the treatment of choice, however we don’t always have those luxuries. What inotrope(s) do we use in cariogenic shock? How do we approach those patients for the best outcome?
 Choosing the right vasopressor agent in hypotension
Choosing the right vasopressor agent in hypotension
The majority of evidence comparing pressors head-to-head has been done in patients with septic shock; the largest amount of data has compared high-dose dopamine to norephinephrine. Based on this data, norepinephrine has been associated with lower incidence arrythmias and improved mortality when compared to dopamine. Epinephrine has been compared with several other regimens both in septic shock and undifferentiated shock. When epinephrine was compared to norepinephrine and dobutamine, all of the agents were equally effective in achieving hemodynamic goals, though epinephrine was associated with increased incidence of tachydysrhythmias and prolonged metabolic derangement when compared to other agents. There was no difference in mortality. Robust data comparing other similar agents in other disease processes are lacking.
 Emerging Updates in Septic Shock
Emerging Updates in Septic Shock
In the care of patients with sepsis and septic shock, Norepinephrine (levophed) is the vasoactive medication of choice. The use of Norepinephrine as a first-line agent in septic shock is supported by both the SSc, as well as the CAEP consensus guidelines on vasopressor and inotrope use in the Emergency Department. But what happens in the patient with persistent shock despite high doses of norepinephrine? Second-line recommendations are not as clear.
 High dose vasopressors: Never surrender
High dose vasopressors: Never surrender
The concept of a “maximum dose” of vasopressors should be discouraged, as this appears to be a myth. Limiting vasopressor dosage below an arbitrary rate could prevent successful resuscitation of the sickest patients.
 Occult Causes of Non-Response to Vasopressors
Occult Causes of Non-Response to Vasopressors
The cognitive response to hypotension should not be reaching for a pressor. The primary therapy for any sick hypotensive patient is treatment of the underlying pathology.
 Peripheral Vasopressor Infusions and Extravasation
Peripheral Vasopressor Infusions and Extravasation
So can we use peripheral lines for vasopressors? Folks like my friend Paul Mayo would say, “yes!” In his unit, pts are getting peripheral or mid lines almost exclusively. 10 mg of Phentolamine can be added to each liter of solution containing norepinephrine. The pressor effect of norepinephrine is not affected.
 Peripheral Vasopressors: Safe or Dangerous?
Peripheral Vasopressors: Safe or Dangerous?
Clinical Take Home Point: In patients with shock, use of peripheral vasopressors (Norepinephrine and Dopamine) in a large bore IV (18 – 20g) at a proximal site (antecubital fossa or more proximal) run for ≤4hrs or less is a safe option until more central access can be achieved.
 Pressors for Hemorrhagic Shock
Pressors for Hemorrhagic Shock
AVERT trial shows vasopressin decreases transfusion requirements.
 Vasopressors in 2022
Vasopressors in 2022
This is a work-in-progress blog post on vasopressors.
Vasopressors in the ED
Our body has 3 major classes of vasopressors - Catecholamines - ⍺/β receptor agonism - Vasopressin – Vasopressor receptor (V1) agonism - Angiotensin II – Angiotensin II Receptor (ATII-R) agonism
Vasoactive Drips: A guide to starting and titrating critical care drips, Adult and Pediatric
Vasopressors should be infused via central access but can be administered peripherally until central access is obtained. All vasoactive drips can cause severe tissue injury if infiltration occurs.
An alternative viewpoint on phenylephrine infusions
There is a misconception that norepinephrine is dramatically different from phenylephrine. However, the pharmacology of these drugs is similar. Norepinephrine is equivalent to phenylephrine plus a bit of beta-stimulation.
An update on peripheral vasopressors
We have new evidence looking at the use of vasopressors through a peripheral IV.
Are central lines really needed for vasopressor infusions?
If these authors' findings are replicated in a multicenter trial, we may one day conclude the risk of tissue injury from careful peripheral administration of vasopressor is lower than the combined (also low) risks of pneumothorax, arterial puncture, and bacteremia associated with central venous catheterization.
Are Peripheral Vasopressors Safe?
It is important to remember that the use of peripheral vasopressors is a bridge to something else and not prolonged infusions. This would either mean the patient improves and comes off vasopressors or does not improve in which case a CVC should be placed.
EMCrit RACC: Podcast
Vasopressor Basics
Peripheral vasopressors: the myth and the evidence
The myth: It is an absolute contraindication to administer vasopressors through a peripheral intravenous line. Although this is probably a myth, it is important to be clear: vasopressors can cause tissue damage after extravasation.
Podcast 642: Vasopressors
Educational Pearls...
Pressors in cardiogenic shock
Norepinephrine is considered first-line in cardiogenic shock with profound hypotension (SBP < 70 mm Hg)...
Tasty Morsels of Critical Care 043 | Inotropes and vasopressors
First off our beloved catecholamines. There are typically our first line in the fight against MAP<65. We have a fairly bewildering range of options available to us all with their own nuances.The nuances stem from the variety of catecholamine receptor biology we have evolved over the millenia. We know the basics of α and β but these can be extensively sub divided further in forms that only reinforces how little I understand about medicine despite over 20 years studying it.
The Vasopressor Toolbox for Defending Blood Pressure
The first-line treatment for hypotension remains volume resuscitation, but the addition of vasopressor therapy may be required to achieve hemodynamic goals. Norepinephrine remains the most commonly used vasopressor for the treatment of hypotension in septic shock.1,2 The vasopressor “toolbox” has other potent pharmacologic interventions as well. Other vasopressors, including dopamine, epinephrine, phenylephrine and vasopressin, can be used in combination with, or instead of, norepinephrine based on patient-specific parameters for different clinical indications, mechanism of action or adverse effects.
To Push or Not to Push? Vasopressors Outside the Operating Room
Vasopressor agents are typically administered as continuous infusions. However, bolus doses of vasopressors have been used to optimize a patient’s hemodynamic status when rapid intervention is required. This method of intermittently administering bolus vasopressor doses can be referred to as push-dose vasopressors, neo-sticks, or phenyl-sticks.
Under Pressor! Utilizing IV pressors in the emergency department
In the case of pulmonary embolus or shock with acute pulmonary hypertension, Dr. DeBlieux said the best vaso-active agent is norepinephrine. Although there is no human data, limited animal studies support that norephinephrine is associated with improved survival, improved cardiac output and coronary blood flow, and minimal changes in pulmonary vasculature. “Be cautious with fluid application,” he said. Norepinephrine is also the agent of choice for patients in septic shock,
Vasopressors for septic shock
Vasopressors should be promptly begun in patients in persistent septic shock despite fluid resuscitation; vasopressors can be begun and continued simultaneously with fluid resuscitation, especially in patients with severe hypotension.
Vasopressors – When and Why
Discusses the clinical situations when to use specific vasopressors...
 Peripheral Vasopressors – Are my days of Placing Central Lines Over? Not Yet?
Peripheral Vasopressors – Are my days of Placing Central Lines Over? Not Yet?
You have undoubtedly heard some discussion about data coming out over the last couple of years suggesting the risk of running vasopressors via peripheral IV's is less than we previously thought. Well I'm here to tell you: don't let your central line skills erode just yet. While new studies that change our practice are exciting, we must be careful not to be early adopters after reading just the headlines.
EMCrit Project
Good review of vasopressors...

Introducing Stitches!
Your Path to Meaningful Connections in the World of Health and Medicine
Connect, Collaborate, and Engage!
Coming Soon - Stitches, the innovative chat app from the creators of HWN. Join meaningful conversations on health and medical topics. Share text, images, and videos seamlessly. Connect directly within HWN's topic pages and articles.













