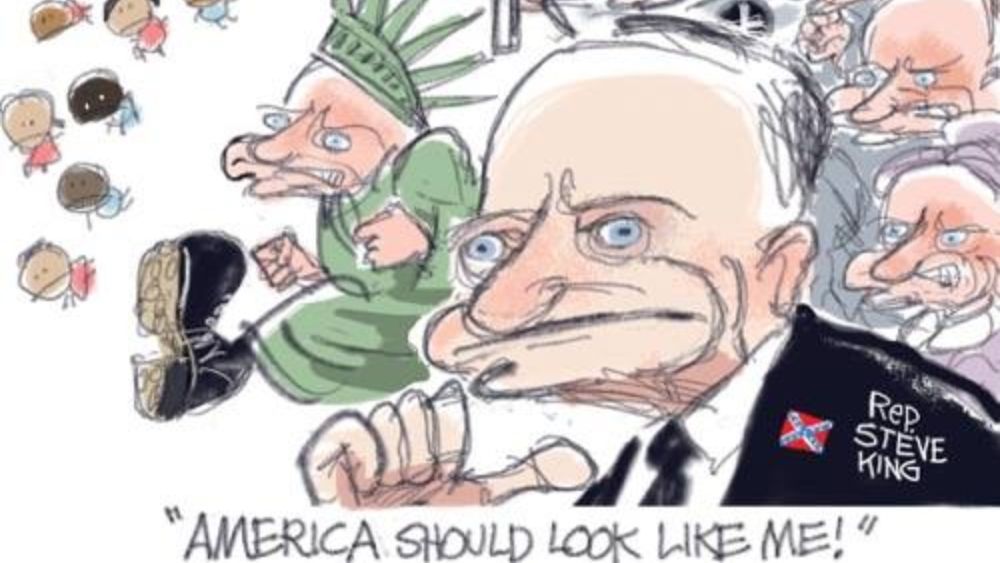
Can Heartburn Cure AFib? Maybe!
Shilo Zylbergold | Best Medicine
.jpg)
image by: Jodi K Johnson
Don’t let anyone, especially your doctor, tell you that A-Fib isn’t that serious, or you should just learn to live with it - Steve S. Ryan
This heart of mine has been misbehaving again. I say “again” because I’ve been forced to deal with arrhythmia for over forty years. My particular condition is called atrial fibrillation and over the years I have battled against this debilitating affliction with beta blockers, blood thinners, and even a surgical procedure called a pulmonary vein ablation.
Everything I’ve tried has worked just long enough for me to believe that I’ve been healed, and then I have had my bubble burst over and over again by treatment failure.
This time was going to be different. I had been told by my electrophysiology cardiologist that the technology had vastly improved over the dozen years since my previous ablation. Back then it took only two years before I was fibrillating again and had to be put back on drugs to control the condition.
So there I found myself, on a surgical trolley being wheeled into the operating room. The last thing I remember before passing out from the anesthetic was looking up at my team of nurses, cardiologists, and anesthetist and noting how they all looked like middle school students to this septuagenarian.
Briefly, the procedure involves passing tubes up from an insertion point on my right groin area up to the left atrium of the heart. A catheter capable of creating destructive burns follows this pathway up into the heart. After several hours of surgery, all the internal parts which have been interfering with the regular heart rhythm are eliminated or neutralized and the surgical equipment is withdrawn.
I came to in the recovery room where I had to spend the next four hours lying flat on my back while a number of sandbags were applied firmly to the entry point wound on my groin in order to stop any possibility of post-surgery bleeding. I found this part of the ordeal the most disturbing and even excruciating as I was restricted from moving into any other position for the entire time.
Finally, after being taken for a test walk around the recovery room, I was ready to be sent back out into the world. Before being discharged, I had a quick consultation with my cardiologist, even though my brain was still floating several inches above my head due to the aftereffects of my anesthetic. My doctor warned me not to expect perfect heart rhythm after the ablation procedure. After all, I had just been subjected to between 50 to 70 burns to areas in my heart, a number of big tubes inserted in my veins, hours of confined bed rest, and dubious anesthetics pumped through my system. Although I felt like this was synonymous to being told by your auto mechanic, after you’ve taken your car in for repairs, to not expect your car to stop every time when you hit the brakes, I nodded my head at the doctor in agreement.
The main message my doctor wanted to impart to me was that an atrial fibrillation ablation was a “big deal”. There were a number of complications I could expect over the next few weeks. Those burns that were delivered using standard radio frequency catheters could possibly result in chest pain especially when taking a deep breath or while coughing (a result of the irritation to the lining of the heart or pericardium). As well, the general anesthesia effects could leave me with nausea and groggy symptoms for a few hours or days. I could also expect a sore throat and lingering cough resulting from the endotracheal tube which had been used during surgery. I must admit, at this point I was wondering whether it might have been better to have just tried to tolerate the arrhythmia than having to deal with all this “new stuff”.
As they say in K-Tel t.v. ads, “but that’s not all, folks!” There were a few more obstacles I had to dodge before I could consider myself on the road to recovery. One of the main culprits was the entry point in the right groin where the sheaths and catheters were inserted. It was quite normal for a small lump to form there at the puncture site, but it would likely shrink and eventually disappear with time. Not only could there be pain and tenderness at this point, but there could be a resulting injury to the vein or artery. I could also expect some degree of bruising as black and blue marks would follow gravity down my leg. I tried to look on the bright side. Maybe this would save me some money I would otherwise have spent on tattoos.
I was beginning to realize that my heart was going to be pretty “pissed off” with me over the next while for what I had just inflicted on it. The prolonged bed rest, the effects of the anesthesia, and the accompanying pain were likely to trigger short bouts of arrhythmia, which is what I was trying to escape in the first place. My heart rate was likely to go up by a few beats per minute, but if it stayed persistently high, then it might indicate left atrial flutter which would be more difficult a problem requiring possible cardioversion or zapping of the heart with an electric shock.
Apparently, although post procedure atrial fibrillations can often occur, they are not that dangerous due to the fact that the possibility of strokes is minimized by keeping patients on anti-coagulation and rate-slowing meds.
I was also sent away with some printed literature that outlined what I could expect in the next few days and weeks. There was a list of “do’s and don’ts” as well as a number of activities I should avoid while recovering. Foremost among these restrictions was that I was not allowed to drive for the next 24 hours as I was considered impaired. Duh. I could barely place one foot in front of the other without teetering over to one side so there was no way I needed to be told that I was a driving risk.
Along the same lines, I was told not to operate heavy machinery in the next few days. Too bad, because I had my heart set on getting behind the controls of a high-rise construction crane early the next morning.
What else was on the restricted list? No alcohol, anxiety drugs, or sleeping pills. Refrain from making big decisions or signing important papers. I was, under no circumstances, to be responsible for another person or child, so that pretty much killed any plans for my packing parachutes for a sky diving adventure.
Two of the more immediate 24 hour no-no’s were stair climbing and sexual activity, both as individual workouts or combining them by getting it on in a stairwell.
The list went on. I was to do no jogging, cycling, swimming or lifting of any weight over ten pounds. As well, for the next two days, I was instructed to avoid kneeling, crouching or sitting for more than an hour. For
So what are recuperating ablation patients supposed to do with their time? Seriously, you can only spend so much time drooling while standing in front of the fridge with the door open. Luckily, there was more useful advice listed on the printout from the Atrial Fibrillation Clinic that was handed to me upon discharge from the hospital. Take a few weeks off, it suggested. Read books, watch movies, write a blog. I imagine I was supposed to go light on political thrillers and horror genre films that were guaranteed to give my heart a workout that was equivalent to stairwell sex.
It has now been about five weeks since my pulmonary vein ablation surgery. I’ve been told that it takes between six to ten weeks before it can be determined whether the procedure was a success or not. The success rate for my particular pattern of atrial fibrillation ranges between 60- 70%. Because this is now my second go around with the procedure, my chances are even better: above 80%. In the meantime, I have experienced two major bouts of arrhythmia with accompanying very elevated heart rates. Each one lasted approximately 12 hours and really sent me for a loop. They did however clear up spontaneously without any medical intervention.
I have my fingers crossed that the odds will be with me and that I might not have to deal with arrhythmia and the associated dangers of stroke ever again. In the meantime, I’m staying out of stairwells.
Introducing Stitches!
Your Path to Meaningful Connections in the World of Health and Medicine
Connect, Collaborate, and Engage!
Coming Soon - Stitches, the innovative chat app from the creators of HWN. Join meaningful conversations on health and medical topics. Share text, images, and videos seamlessly. Connect directly within HWN's topic pages and articles.








.jpg)